Aim: Globally measure the effect of the health care system in terms of years lived in good health.
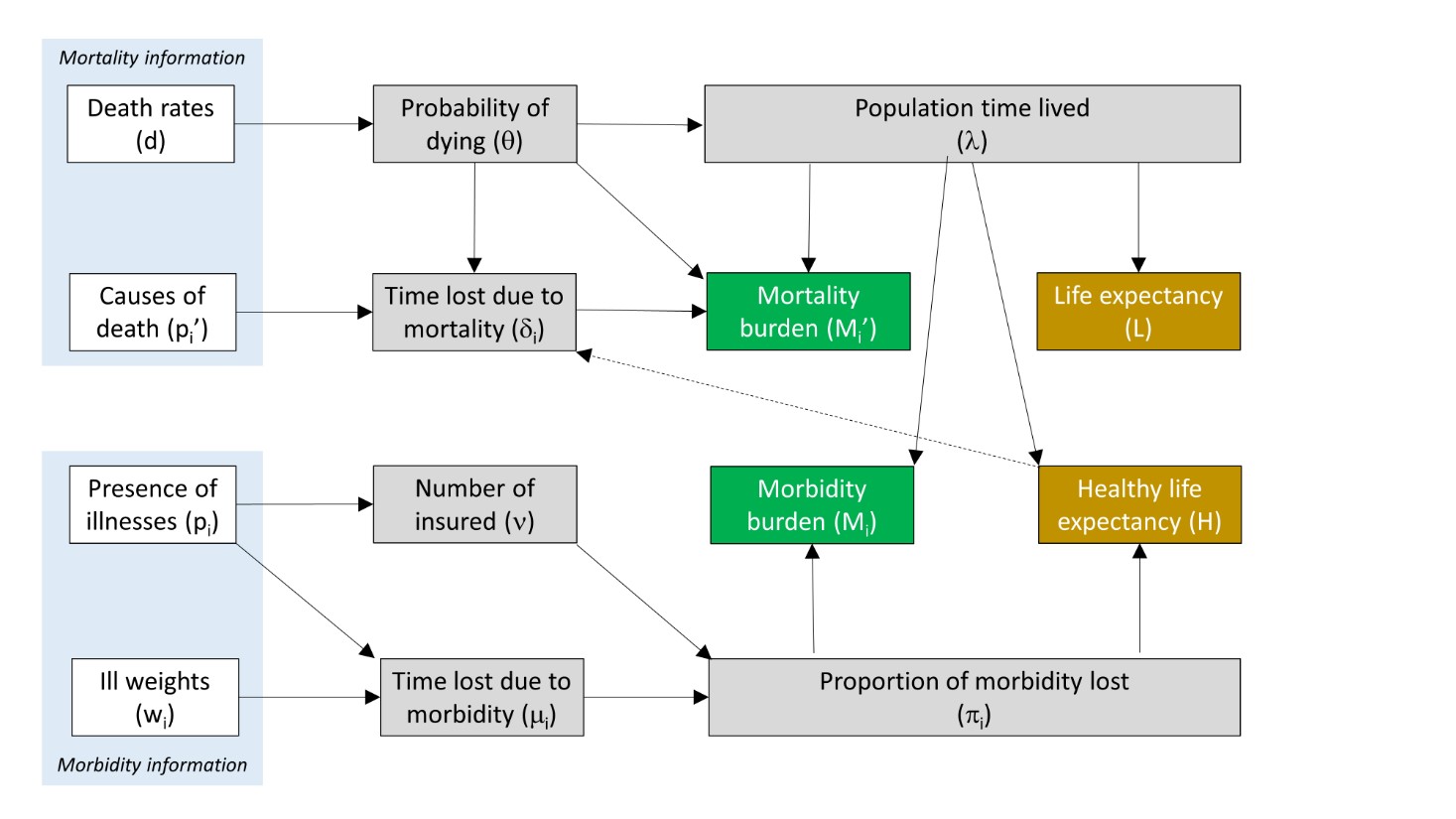
Mortality burden: Time lost due to death, corresponding to the healthy life expectation at the age of dying. Example: 20 years for a 60 years old man dying.
Morbidity burden: Time lost due to illness, corresponding to the number of disability days during the year divided by 365. Disability days depend on the consumption of health services. For instance, a person receiving 80 nurse visits, visiting 11 times a physician, and spending three days at the hospital (amounting to 9 disability days) has 100 disability days among 365, i.e. a disability of 0.3 during the year.
Data sources: Mortality information is available from demographic statistics and death registries (Swiss federal office of statistics).
Morbidity information is retrieved from insurance data (medical statistics if available, prescribed drugs).
Life expectancy: Life expectancy is calculated from the survival years of a cohort of 100’000 people, applying probabilities of dying at each year of life by gender.
Health life expectancy: Health life expectancy is calculate from survival years after deduction of the morbidity burden for each year of life. It depend on the proportion of morbidity lost for each year of life, weighted by the population time lived (survivors at each year of life).
Strength of the indicator: The indicator combines information from death registries and insurances from a specific year. It is thus also highly reactive to time or regional variations. The result depends on objective data and, thus, is less biased than healthy life expectancy based on subjective inquiries. Contrarily to other indicators like DALYs, it does not depend on the structure of the population. The mortality and morbidity burdens can be allocated by age, gender and diseases, offering the opportunity to test the efficiency of public health measures (prevention and treatment programs) with specific focus (e.g. by age, by risk factor, etc.).
Limitations: Some people suffer from diseases without consuming health services (hemiplegic or blind patients for instance). Moreover, two populations with the same health status might have different level of health services consumption because of a differential in the access to health facilities. Nevertheless, most severe conditions lead to health services consumption, and it does not matter if there are some substitution between different types of service (hospital, outpatient, medico-social). Ideally, it would be desirable to combine morbidity information from several sources (insurance data on drugs’ prescriptions, hospital data, and cancers’ registries).